This silent lung infection is on the rise. Discover the key symptoms and high-risk zones to protect yourself and your family.
Did you know that a simple gust of wind in certain parts of California could carry a hidden health threat? It’s an airborne fungus that causes an illness known as Coccidioidomycosis, but you probably know it by its more common name: Valley Fever. While it might sound like a localized problem from a bygone era, this respiratory infection is a growing concern across the Golden State, with climate change and development potentially expanding its reach into 2025 and beyond.
Many early cases of Valley Fever are dismissed as a common cold or the flu, leading to delayed diagnosis and, in some instances, severe health complications. Understanding what this disease is, recognizing its unique symptoms, and knowing which areas pose the highest risk are critical for your health and safety.
In this definitive guide, we’ll uncover everything you need to know about Valley Fever in California. You’ll learn:
-
What causes this fungal infection.
-
The full spectrum of symptoms, from mild to severe.
-
An updated look at the high-risk zones in California for 2025.
-
Effective treatment options and crucial prevention strategies.
-
Answers to your most pressing questions about this misunderstood illness.
Let's dive in and demystify the dust.
3. Table of Contents
-
What Exactly is Valley Fever? A Simple Explanation
-
The Fungus Behind the Fever: Coccidioides
-
How Do You Get Valley Fever? The Path of Infection
-
-
Recognizing the Symptoms: Is It Valley Fever or Something Else?
-
Common, Flu-Like Symptoms
-
When to Worry: Severe and Disseminated Valley Fever
-
The "Great Imitator": Why It's Often Misdiagnosed
-
-
High-Risk Zones in California for 2025: An Updated Map
-
The Traditional Hotspots: Central Valley and Southern California
-
Emerging Areas of Concern: Why is it Spreading?
-
Climate Change and its Impact on Valley Fever Spores
-
-
Who is Most at Risk? Identifying Vulnerable Populations
-
Age, Occupation, and Pre-existing Conditions
-
Are Pets at Risk Too? Protecting Your Four-Legged Family
-
-
Getting a Diagnosis: From Symptoms to Certainty
-
The Diagnostic Process: Blood Tests and Imaging
-
The Importance of Early Detection
-
-
Treatment Options for Valley Fever
-
For Mild Cases: Rest and Monitoring
-
Antifungal Medications: When and Why They Are Used
-
Managing Long-Term Complications
-
-
Prevention is Key: How to Reduce Your Risk
-
Practical Tips for a Dust-Free Environment
-
Precautions During High-Risk Activities
4. Main Body Content
What Exactly is Valley Fever? A Simple Explanation
Before we can fight it, we need to understand it. Valley Fever isn't caused by a virus or bacteria like the flu or strep throat. It’s a fungal infection, and its journey from the soil to your lungs is a fascinating, if not unsettling, process.
The Fungus Behind the Fever: Coccidioides
The culprit is a microscopic fungus called Coccidioides (kok-sid-ee-oy-dees). There are two nearly identical species that cause the illness: Coccidioides immitis and Coccidioides posadasii. This fungus thrives in the arid and semi-arid soils of the southwestern United States, Northern Mexico, and parts of Central and South America. In California, it is particularly prevalent in the Central Valley region—hence the name "Valley Fever."
In the soil, the fungus exists in a long, filamentous form. But when the soil is disturbed by wind, construction, farming, or even an earthquake, it breaks into tiny, lightweight spores that become airborne.
How Do You Get Valley Fever? The Path of Infection
Infection occurs when a person inhales these microscopic fungal spores. It's that simple. You don't get it from another person or an animal; it is not contagious.
Once inside the lungs, the warm, moist environment allows the spores to change form and multiply. The body's immune system typically rushes to fight the invaders, and for about 60% of people, this battle happens without them ever feeling sick. For the other 40%, the fight triggers the symptoms we recognize as Valley Fever.
Recognizing the Symptoms: Is It Valley Fever or Something Else?
One of the biggest challenges with Valley Fever is that its early symptoms mimic many other common respiratory illnesses. This often leads to misdiagnosis, with doctors initially suspecting community-acquired pneumonia or influenza.
Common, Flu-Like Symptoms
If symptoms do appear, they typically start one to three weeks after exposure. The most common signs include:
-
Fatigue (often severe and long-lasting)
-
Cough (usually dry)
-
Fever
-
Shortness of breath
-
Headache
-
Night sweats
-
Muscle aches or joint pain
-
A rash on the upper body or legs (can look like red bumps or a blistering rash)
Because these symptoms are so general, it’s crucial to inform your doctor if you live in or have recently traveled to an at-risk area like California's Central Valley.
-
-
When to Worry: Severe and Disseminated Valley Fever
For most healthy individuals, Valley Fever resolves on its own within a few weeks to months, though the fatigue can linger. However, in about 5-10% of cases, the infection can lead to serious, chronic lung problems.
In about 1% of cases, the infection "disseminates," or spreads, from the lungs to other parts of the body. This is a severe and potentially life-threatening complication. Disseminated Valley Fever can affect:
-
Skin: Sores and ulcers
-
Bones and Joints: Swelling and intense pain
-
Central Nervous System: Can lead to fungal meningitis, a serious infection of the membranes surrounding the brain and spinal cord.
The “Great Imitator”: Why It’s Often Misdiagnosed
Because its symptoms overlap with so many other conditions—from bacterial pneumonia to lung cancer—Valley Fever has earned the nickname "The Great Imitator." A study by the [External Link: CDC] found that delays in diagnosis are common. If you have persistent flu-like symptoms and have been in an endemic area, actively asking your doctor, "Could this be Valley Fever?" could be life-changing.
High-Risk Zones in California for 2025: An Updated Map
Knowing where the Coccidioides fungus lives is the first step in protecting yourself. While it's most famous for inhabiting the Central Valley, its territory is expanding.
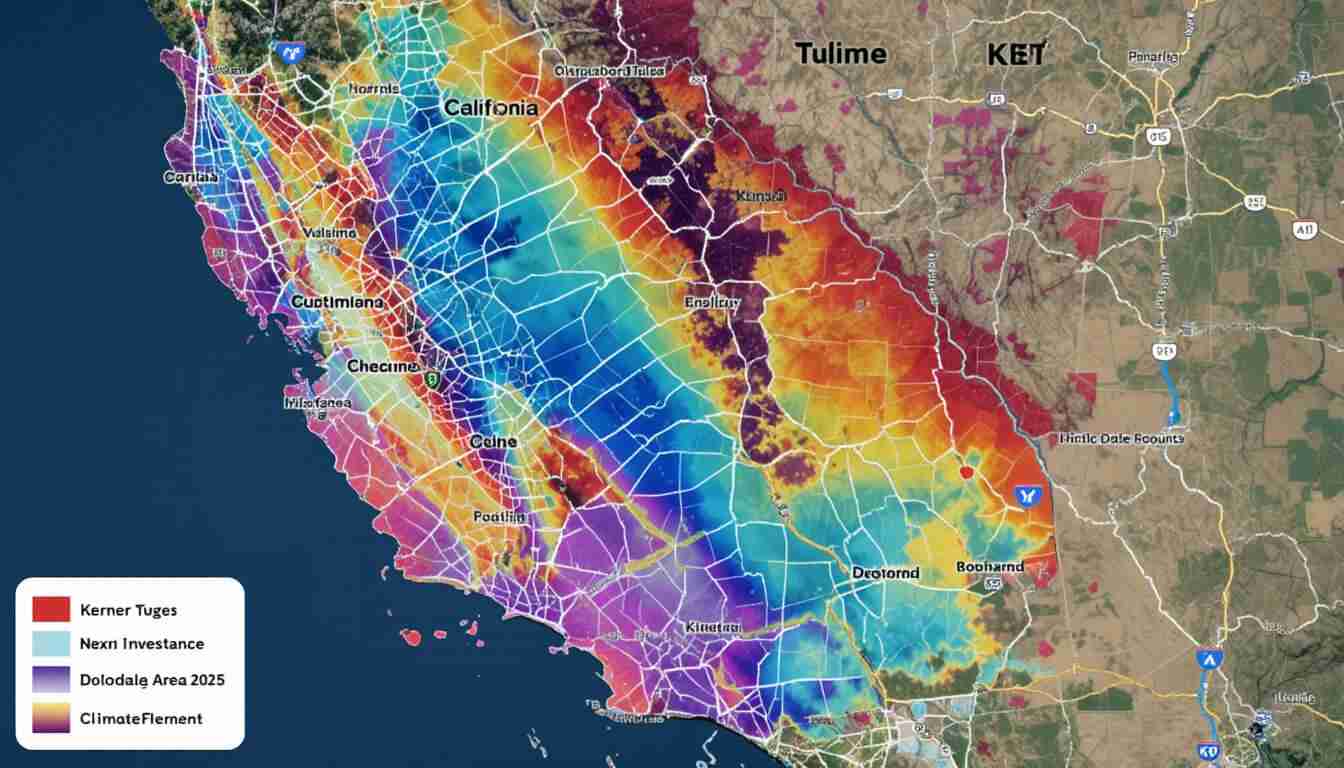
The Traditional Hotspots: Central Valley and Southern California
Historically, the highest-risk counties have been in the southern half of the Central Valley. These include:
-
Kern County (often considered the epicenter)
-
Kings County
-
Tulare County
-
Fresno County
-
San Luis Obispo County
Other parts of Southern and Central California, including areas in Los Angeles, Ventura, San Bernardino, and Riverside counties, also report significant cases. For the most up-to-date case numbers, refer to the [External Link: California Department of Public Health (CDPH) Data].
Emerging Areas of Concern: Why is it Spreading?
Here's the critical update for 2025 and beyond: Valley Fever is no longer confined to these traditional zones. Cases are now being reported with increasing frequency in Northern California, including Sacramento, Contra Costa, and San Joaquin counties.
There are a few theories why:
-
Climate Change: Warmer, drier conditions create more dust. More extreme weather patterns, from droughts to intense rainy seasons (which can promote fungal growth), can create perfect conditions for spores to spread.
-
Population Growth and Development: As California's cities expand into previously undisturbed desert and arid landscapes, construction and soil disruption kick up dormant spores, exposing new populations.
The bottom line? The map of where you can get Valley Fever is being redrawn. Even if you don't live in a "hotspot," be aware of the risk, especially during windy, dusty conditions.
Who is Most at Risk? Identifying Vulnerable Populations
While anyone who inhales the spores can get sick, certain groups are more susceptible to developing the severe, disseminated form of the disease.
Age, Occupation, and Pre-existing Conditions
Key risk factors include:
-
Weakened Immune Systems: People with HIV/AIDS, those on immunosuppressive drugs (like after an organ transplant or for autoimmune diseases), and cancer patients undergoing chemotherapy are at highest risk.
-
Race and Ethnicity: For reasons that are still being studied but are likely genetic, Filipinos, African Americans, and Hispanics are more likely to develop severe Valley Fever.
-
Pregnant Women: Women in their third trimester are more vulnerable.
-
Seniors: Individuals over 60 often have a harder time fighting the infection.
-
People with Diabetes: This condition can compromise the immune response.
-
Certain Occupations: Farmers, construction workers, archaeologists, and anyone working with soil in endemic areas have a higher rate of exposure.
Are Pets at Risk Too? Protecting Your Four-Legged Family
Yes, your pets—especially dogs—are also highly susceptible to Valley Fever. Their tendency to dig and sniff the ground puts them at a high risk of inhaling spores. Symptoms in dogs are similar to humans: coughing, fever, lethargy, and lack of appetite. If you live in a high-risk area and your dog shows these signs, mention Valley Fever to your veterinarian. Check out our Frank Caprio Announces Health "Setback" in Brave Cancer Battle Update for more information.
Getting a Diagnosis: From Symptoms to Certainty
If you suspect you have Valley Fever, prompt medical attention is key. A timely diagnosis prevents unnecessary antibiotic use (which don't work on fungi) and ensures you get the right care.
The Diagnostic Process: Blood Tests and Imaging
Your doctor will likely use a combination of methods:
-
Blood Test (Serology): This is the most common diagnostic tool. The test looks for antibodies your body produces to fight the Coccidioides fungus. It can sometimes take weeks for antibodies to be detectable, so a retest may be needed.
-
Chest X-ray or CT Scan: Imaging can reveal abnormalities in the lungs, such as nodules or cavities, that are characteristic of the infection.
-
Biopsy: In some cases, a small sample of tissue from the lungs or another affected area may be taken and examined for the fungal spherules.
The Importance of Early Detection
Early diagnosis helps manage symptoms and significantly reduces the risk of the infection progressing to a severe or disseminated state. It provides peace of mind and puts you on the correct path to recovery, which often involves rest rather than ineffective medications.
Treatment Options for Valley Fever
Treatment for Valley Fever depends entirely on the severity of your illness and your overall health.
For Mild Cases: Rest and Monitoring
Most healthy people with a primary pulmonary (lung) case of Valley Fever don't require specific medication. The body’s immune system successfully contains the fungus. The treatment plan typically involves:
-
Rest: The fatigue can be profound and may last for months.
-
Symptom Management: Over-the-counter pain relievers and fever reducers.
-
Close Monitoring: Regular check-ups with your doctor to ensure the infection doesn't worsen or spread.
Antifungal Medications: When and Why They Are Used
For severe lung infections, or for anyone with disseminated disease, long-term treatment with antifungal medication is necessary.
-
Common Antifungals: The most commonly prescribed drugs are fluconazole (Diflucan) and itraconazole.
-
Duration: Treatment typically lasts for 3 to 12 months but can be lifelong for those with disseminated disease, particularly meningitis.
-
Purpose: These drugs don't "kill" the fungus but rather control its growth, giving the immune system the upper hand.
It’s essential to complete the full course of medication as prescribed by your doctor to prevent a relapse.
Prevention is Key: How to Reduce Your Risk
Since there is currently no vaccine for Valley Fever, prevention is all about minimizing your exposure to airborne dust in endemic areas.
Practical Tips for a Dust-Free Environment
-
Stay Indoors: Avoid being outside during dust storms or on particularly windy days.
-
Keep Windows Closed: Use air conditioning instead of opening windows during high-risk seasons (typically the dry, hot months).
-
Use Air Filtration: High-efficiency particulate air (HEPA) filters can help remove fungal spores from indoor air.
-
Wet the Ground: Before digging or doing yard work, spray the soil with water to keep dust down.
-
Cover Open Soil: Use ground cover, grass, or gravel to reduce exposed dirt around your home.
Precautions During High-Risk Activities
If you work in construction, agriculture, or enjoy hobbies like gardening or off-roading, take extra precautions:
-
Wear a Mask: Use an N95 respirator mask to filter out spores when working in dusty conditions. A simple cloth or surgical mask is not effective.
-
Clean Up: After spending time in dusty areas, wash your hands and face thoroughly, and change your clothes before going inside.
2. Can you get Valley Fever more than once?
It is extremely rare. For the vast majority of people, recovering from a Valley Fever infection provides lifelong immunity.
3. How long does Valley Fever last?
A mild case of Valley Fever can last for a few weeks to a few months. However, the associated fatigue can persist for much longer. Severe or disseminated cases require long-term antifungal treatment, sometimes for life.
4. Is there a vaccine for Valley Fever?
Currently, there is no human vaccine available. However, researchers are actively working on developing one. A vaccine for dogs is also in the pipeline, which could be a significant breakthrough in veterinary medicine.
5. How deadly is Valley Fever?
For most people, Valley Fever is not deadly. The mortality rate is very low, with fewer than 1% of infected people developing the severe, disseminated form. However, for those with weakened immune systems who develop disseminated disease, it can be fatal if not treated aggressively.
Valley Fever is more than just a regional curiosity; it’s a significant and growing public health challenge for California. As our climate and landscapes change, the risk of inhaling Coccidioides spores is becoming a reality for more and more people.
The key to staying safe is awareness. By understanding the flu-like symptoms, recognizing the high-risk zones, and taking simple preventative measures against dust, you can dramatically reduce your risk. If you do feel unwell and suspect an exposure, don't hesitate to advocate for yourself in a medical setting by asking, "Could my symptoms be caused by Valley Fever?"
Empowering yourself with this knowledge is the most effective defense you have against this silent threat from the soil.
What's your experience with Valley Fever? Share your story or questions in the comments below to help our community stay informed. Don’t forget to share this article with your friends and family in California!
The team at Care and Prayer is dedicated to providing clear, reliable, and actionable health and wellness information. We leverage expert insights and data-driven research to help you navigate complex topics and live a healthier, more informed life.
